Quality measurement of health services has relied heavily and almost exclusively on what can be gleaned from administrative data, largely registration/enrollment information and claims.
Efforts to benefit optimally from those information sources have been hampered by the frequent absence of some patient demographic data such as race and income, and from billing patterns that are intended to maximize reimbursement rather than information. On occasion, chart audits are done that provide additional data, but this approach is usually intended to validate billing claims.
There is some optimism that widespread adoption of electronic medical records will allow much more detail about clinical presentation and management, though in the foreseeable future, use of this capacity for quality assessment is likely to be limited to large health care systems with interoperable information technology.
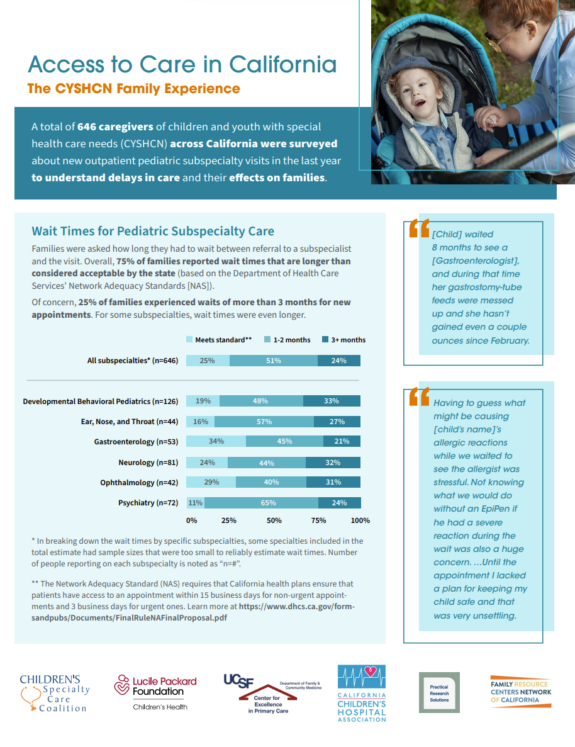
To measure the quality of care for children with chronic or complex health conditions, the heterogeneity of their conditions generally precludes use of disease-specific quality measures. Instead, population health measures that assess functional health status, family health and well-being, health-related behaviors, integration into communities, and achievement of health-related goals are more feasible.
Such data on patient experiences are viewed by some as the most valuable information by which to assess quality, but these data are especially difficult to obtain. The difficulty is usually described in terms of the additional costs involved in surveying patients. Consequently, patient experience data are most often collected as part of special projects rather than as a routine component of quality assurance activities. It is time for that “special status” of patient experience measurement to change, and for its assessment to become an integral part of health care services.
Patients’ and families’ experiences can be ascertained through consumer advisory committees, focus groups, discharge interviews, and surveys done in real time or retrospectively using a variety of media. The choice of modality may reflect the questions being asked and the entity asking, e.g., government programs, insurers, health plans, hospitals, or health care providers. Regardless of the approach, the costs of assessing patients’ experience should be treated as just another cost of routine health care, not as something special that is added onto usual costs.
Patients and families should come to expect to give feedback and expect for it to be thoughtfully considered. There are good business reasons to listen to customers, evidence that it can be cost saving, and strong arguments for consistently engaging patients as partners not only in their own care, but as partners in improving the health care system for others.