What do primary care pediatricians really want and need to best care for their young patients with special health care needs? Kris Calvin, CEO of the American Academy Of Pediatrics-California District, is finding out with a grant from the Lucile Packard Foundation for Children’s Health.
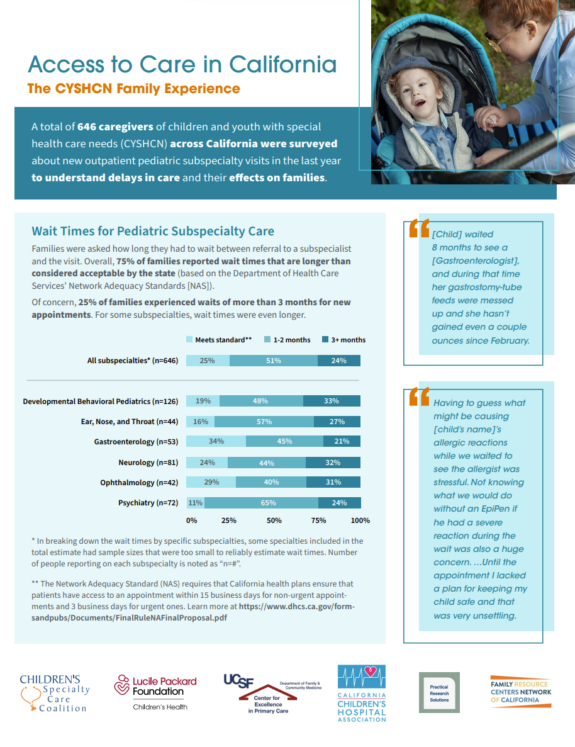
While most children only need to see a pediatrician for well-child visits and the occasional illness, children with special health care needs pose a singular set of challenges for non-specialist pediatricians. One of the biggest: the largely unreimbursed task of coordinating care with specialists and other care providers, including educators and mental health professionals.
In the past, questions have – appropriately – been aimed at families about what works for them in caring for children with special health care needs, Calvin said. Now, Calvin, a health economist by training, is asking pediatricians for their ideas about what would make systems of care work better for families and children – and for the pediatricians themselves.
Through in-depth interviews with more than 30 pediatricians and a forthcoming survey of 3,000 AAP members statewide, Calvin is investigating what pediatricians perceive as their biggest barriers and supports to providing the best care for children with special health care needs. The survey results are expected by March 2014.
“Many primary care pediatricians find a higher volume of patients to be a necessity to survive in practice,” Calvin said. “They are struggling with how to make the time in a high-volume practice to provide the care coordination that children with special health care needs require, particularly when time spent on coordination is not reimbursed by insurers.”
These concerns, Calvin said, are underscored by ongoing worries about low reimbursements from insurers, including Medi-Cal, for medical care in general.
Calvin is finding that community pediatricians who are early in their careers and work in larger practices or integrated health systems appear to be more comfortable in providing care coordination, while others believe medically complex children are best served if their medical home is with a university-based pediatrician who may have easier access to specialists.
And, she said, a majority of pediatricians say that while improving reimbursement for care coordination is important, educating families to help coordinate care for their children is also critical.
“The better prepared and supported a family is to coordinate their child’s care,” Calvin said, “the better job a doctor can do.”